At ProImpact, we believe in educating our patients and their parents / caregivers on their particular injury. On this page, you will find articles that were carefully and purposefully selected. We feel each article clearly explains the topic being discussed and hope you will agree.
Each category is specific to the general area of the body. Within each category, you will find subcategories that list case studies specific to various injuries. Links to the full articles and their websites are listed in addition to the information provided.
Shoulder
-
Adhesive Capsulitis (Frozen Shoulder)
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“This is a condition characterized by pain and stiffness in the shoulder joint. Sign and symptoms usually begin gradually, and get worse with time. Frozen shoulder is common if you are recovering from an injury or procedure that prevents you from moving your arm.” Mayo Clinic
VIEW IT -
AC Joint Injury
This is information from the Move Forward website; a link to the full article will be linked below.
“An AC joint injury occurs at the top of the shoulder, where the front of the shoulder blade attaches to the collarbone. These injuries can be caused by a traumatic event, such as a fall on the outside of the shoulder, or repetitive overuse. These injuries are most common in athletes that play high collision sports, such as football, biking, snow sports, hockey, and rugby.” Move Forward
VIEW ITHow does this feel?
This information is from the Move Forward website; a link to the full article will be linked below.
- General shoulder pain and swelling
- Swelling and tenderness over the AC joint
- Loss of shoulder strength
- A visible bump above the shoulder
- Pain when lying on the involved side
- Loss of shoulder motion
- A popping sound or catching sensation with movement of the shoulder
- Discomfort with daily activities that stress the AC joint, like lifting objects overhead, reaching across your body, or carrying heavy objects at your side
-
Biceps Tenodesis
This information is from an article on the ShoulderDoc website; a link to the full article will be linked below.
“This is a procedure that is done to treat a partial or full tears in bicep tendons, severe biceps tendonopathy, or biceps instability associated with rotator cuff tears. Bicep Tenodesis involves detaching the LBH from its superior labrum in the shoulder and reattaching it to the humerus bone just below the shoulder. Compared to a tenotomy, this procedure is more complex; however, this avoids the risk of bicep discomfort, weakness, and a possible “Popeye” appearance.”
VIEW IT
-ShoulderDocThe Procedure for bicep tenodesis:
1. A beach chair or lateral position can be used.
2. The arthroscope is place in the posterior portal and a needle is passed from anterior through the biceps tendon. A suture is then passed through the needle, captured with a grabber from the anterior portal and then extracted. This is to ensure the tendon does not drop down the arm when it is cut.
3. After the tendon is marked with a suture, an arthroscopic scissor is then used to cut the tendon from its origin.
4. A small incision is made over the front of the shoulder to reveal the biceps tendon:
5. The biceps sheath surrounding the biceps is opened and the tendon is then delivered out of the wound
6. The tendon is trimmed and a non-absorable suture is place in the top of the tendon. A guide wire and reamer is then used to make a deep bone tunnel in the humerus.
7. The tendon is fixed back into the bone of the humerus with a special interference screwIf you would like to watch an educational animation of the surgery, please click the link below.
VIEW IT -
Brachial Plexus Injury
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“This injury occurs when the nerves that send signals to the arm, shoulder, and hand are stretched, compressed, or torn. They are also known as stingers or burners, and are common in contact sports, such as football. ” -Mayo Clinic
VIEW IT -
Labral Repair Surgery
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“A Shoulder Joint Tear (Glenoid Labrum Tear) is commonly known as a ‘Labrum Tear.’ The shoulder joint has 3 bones: the shoulder blade (scapula), the collarbone (clavicle), and the upper arm bone (humerus). he head of the upper arm bone is usually much larger than the socket, and a soft fibrous tissue rim called the labrum surrounds the socket to help stabilize the joint. The rim deepens the socket by up to 50% so that the head of the upper arm bone fits better. In addition, it serves as an attachment site for several ligaments.”
VIEW IT
– AAOS.orgRisk Factors
Injuries to the tissue rim surrounding the shoulder socket can result from acute trauma or repetitive shoulder motion. Examples of “trauma” induced injury:
- Falling on extended arm
- Direct impact to shoulder
- Sudden pull while lifting
- Violent overhead reach when stopping a fall
If you would like to watch an educational animation of the surgery, please click the link below.
VIEW IT -
MDI of the Shoulder
This information is from an article on the MoveForward website; a link to the full article will be linked below.
“This injury can be defined as generalized laxity (looseness) of the joint due to excessive mobility and joint weakness. It commonly occurs in people who have increased a joint’s movement, or have ceased to exercise the joint over a period of time. It is very common in baseball pitchers and swimmers.”
VIEW IT
-MoveForwardSigns & Symptoms
This information is from the Move Forward website; a link to the full article will be linked below.
- Pain with pushing, pulling, or carrying heavy objects
- Pain when performing an overhead activity
- Pain during or after exercise
- A feeling that the shoulder is “shifting” (including in bed at night)
- Fear of putting the shoulder in certain positions
- Numbness and tingling sensations in the affected arm
- Clicking and popping sensations with movement
- Weakness when performing athletic movements, especially overhead and away from the body
-
Rotator Cuff Repair
This is information from an article written by Brian Cammarota, a Physical Therapist, a link to the full article will be linked below.
“The rotator cuff is actually made up of four muscles that stabilize the ball in the socket (glenohumeral joint) with the most commonly torn muscle being the supraspinatus muscle. The first indication that this muscle is fully torn is patients being unable to raise the arm over his/her head. For example, they will need to “shrug” the shoulder to raise the arm up, and/or they will be unable to hold the arm in the air if your doctor raises it. This is referred to as the ‘Drop Test.'”
VIEW IT
-Brian CammarotaWhen Surgery is Advisable
Your doctor will know and advise when surgery for a torn rotator cuff is advisable. If you have sought after secondary treatment and pain has not subsided, or it has gotten worse, surgery might be the only option. Furthermore, if you do things on a daily basis that requires having your arms overhead, your doctor will most likely recommend surgery.
- Symptoms lasting six to twelve months
- Tear larger than 3cm
- Significant weakness / loss of function in shoulder
- Tear caused by an acute injury
-
Shoulder Impingement Signs and Symptoms
This is information from the WebMD website; a link to the full article will be linked below.
“The common symptoms of impingement are difficulty reaching behind the back, pain with overhead use of the arm, and weakness in the shoulder muscles. If tendons stay inflamed over an extended period of time, a rotator cuff tear can occur, causing significant weakness.” WebMD
VIEW ITSigns & Symptoms
This information is from the WebMD website; a link to the full article will be linked below.
- The typical symptoms of impingement syndrome include difficulty reaching up behind the back
- pain with overhead use of the arm and weakness of shoulder muscles
- If tendons are injured for a long period of time, the tendon can actually tear in two, resulting in a rotator cuff tear
- Some people can have rupture of their biceps muscle as part of this continuing impingement process.
-
Myositis Ossificans
Myositis ossificans is a bony growth that can occur in any soft tissue in the body but is most common in muscle. Typically, this develops after deep trauma to the tissue, similar to a deep tissue bruise. When the cells in the body try and heal the tissue, calcified (ossified) tissue is laid down instead of muscle tissue. Myositis ossificans can be felt externally; it will feel like a bundle or a knot in the muscle under the skin.1 Typically, this occurs in larger muscles throughout the body.2 This process may initiate about two weeks after the initial impact. Treatment is necessary for myositis ossificans, because it can limit range of motion if the bone growth progresses.1 There is a less common form of myositis ossificans that is inherited and will cause bony growth in multiple sites.2
Treatment will likely involve stretching to preserve range of motion and prevention tactics to keep the area from being impacted again. Subsequent bruising to the area can make the ossified spot larger. Conservative management, including physical therapy, is the first line of defense for myositis ossificans to maintain muscle integrity and range of motion.1
Images of myositis ossificans can be seen in radiographs provided at the sites below.
VIEW IT VIEW IT -
Shoulder Replacement Surgery
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“When non-surgical treatments fail to adequately treat shoulder arthritis, your physician may recommend shoulder replacement surgery. During surgery, the damaged surfaces of the shoulder joint are removed and replaced with prosthetic parts typically made of durable plastic or metal.”
VIEW IT
AAOS.orgShoulder Replacement and Resurfacing Options
- Total shoulder replacement (traditional shoulder arthroplasty)
- Reverse shoulder replacement (reverse total shoulder arthroplasty)
- Partial shoulder replacement (stemmed hemiarthroplasty)
- Shoulder Resurfacing (resurfacing hemiarthroplasty)
-
Suprascapular Nerve Palsy
The suprascapular nerve innervates the infraspinatus and supraspinatus, which are components of the rotator cuff that respectively externally rotate and abduct the arm. When damage or compression occurs to the suprascapular nerve, the brain is unable to transmit signals to the muscle to contract properly and this presents as weakness. It has been known to occur in individuals who perform a lot of overhead motions or in people with involved rotator cuff tears. Any kind of traction (stretch) or compression to the nerve, however, can cause this kind of nerve palsy. This could include cysts or bone spurs. Typically the compression occurs in scapular notches where the nerve travels.The first line of treatment for suprascapular nerve palsy is typically physical therapy, where you and your therapist will work on neural mobility and strengthening weakened or atrophied muscles. You will retrain the shoulder mechanics to ideally prevent this from occurring again. Surgical options are discussed to remove compression on the nerve from something like a cyst, but may also be considered if the pathology has been occurring for a long time. Surgery may also be an option if there are more tissues involved, like rotator cuff injuries or bony overgrowth.
The first line of treatment for suprascapular nerve palsy is typically physical therapy, where you and your therapist will work on neural mobility and strengthening weakened or atrophied muscles. You will retrain the shoulder mechanics to ideally prevent this from occurring again. Surgical options are discussed to remove compression on the nerve from something like a cyst, but may also be considered if the pathology has been occurring for a long time. Surgery may also be an option if there are more tissues involved, like rotator cuff injuries or bony overgrowth.Physical therapy for suprascapular nerve palsy focuses on gaining or maintaining full active range of motion of the shoulder. This may involve retraining muscles to work synchronously and teaching shoulder biomechanics to ensure the injury does not reoccur, Afterwards, you will begin to strengthen the shoulder girdle to allow you to return to your normal activities.
Physical therapy for suprascapular nerve palsy focuses on gaining or maintaining full active range of motion of the shoulder. This may involve retraining muscles to work synchronously and teaching shoulder biomechanics to ensure the injury does not reoccur, Afterwards, you will begin to strengthen the shoulder girdle to allow you to return to your normal activities.
VIEW IT -
Erb’s Palsy
Erb’s Palsy results from a brachial plexus injury at birth. The brachial plexus supplies the nerves that control the muscles of the shoulder and arm as well as sensation to the upper extremity.1 Typically this injury affects nerves C5 and C6, but may have some involvement at C4. This affects most of the muscles around the shoulder and upper arm. This includes the rotator cuff, deltoid, and bicep.2

During delivery, the baby’s head and neck may get overstretched to one side, causing this injury to the nerves. There are varying degrees of injury that affect how much motion and sensation may be available in the arm, and in many cases, physical therapy can help retrain the affected muscles. Physical therapy completed early and often is the best way to get the maximum possible muscle recovery.2
There are several surgeries that may be available and performed in infancy if the child does not appear to be making progress with physical therapy interventions. The nerve can be surgically altered by grafting another nerve from elsewhere in the body to the brachial plexus, or by transferring donor nerves to help control the muscle.2
VIEW IT VIEW IT -
Calcific Tendonitis
“Calcific tendonitis refers to a build-up of calcium in the rotator cuff (calcific deposit). When calcium builds up in the tendon, it can cause a build up of pressure in the tendon, as well causing a chemical irritation. This leads to pain. The pain can be extremely intense. It is one of the worst pains in the shoulder (the other being Frozen Shoulder ).
In addition to the chemical irritation and presssure, the calcific (calcium) deposit reduces the space between the rotator cuff and the acromion, as well as affecting the normal function of the rotator cuff. This can lead to subacromial impingement between the acromion and the calcium deposit in the rotator cuff when lifting the arm overhead.
The cause of the calcium build-up in the rotator cuff is not known. It tends to be more common in people between the ages of 30-60 years of age. It does eventually disappear spontaneously, but this can take between 5 to 10 years to resolve.” – Shoulder Doc
VIEW IT -
Parsonage-Turner Syndrome
What is it?
Parsonage-Turner Syndrome is a condition in which one feels a sudden onset of sharp, burning, stabbing, and/or throbbing shoulder/upper arm pain along the path of one or more nerves. The pain is followed by progressive atrophy (weakness) in the affected area. The nerves that cause the pain are a network of nerves called the called the brachial plexus which controls the movement and sensation in the shoulders and arms. The pain is usually located on one side of the body but very rarely can extend to, or occur on the other side of the body. The pain is typically constant but will increase with movement or different positions of the body. The sharp, intense pain can last anywhere from a few hours to a few weeks. It then weakens to a more mild pain that can last for up to a year. As stated earlier, as the pain subsides, the affected area becomes very weak, and in some extreme cases, can become almost complete paralysis.
What is the cause?
The cause of Parsonage-Turner Syndrome still remains unknown but researchers believe it is a multifactorial condition. This means that it is caused by both genetic and environmental factors. For example, if someone carriers the right genes for the syndrome, they might never know until they are exposed to an environmental factor. Also, some researchers suspect it originates from an autoimmune response following a viral or bacterial infection or certain triggers. The triggers could be, but are not limited to, surgery, vaccinations, childbirth, certain procedures that involve the use of radiologic dye, strenuous exercise, or an injury. To diagnose Parsonage-Turner Syndrome, doctors usually suspect the syndrome due to the patients symptoms but use tests to rule out similar conditions.
What is the treatment?
The treatment plans varies between patients based-off their specific condition and symptoms, rather than one overarching treatment. To manage the pain, doctors typically recommend a combination of opioids and non-steroidal anti-inflammatory drugs. After the acute phase, the doctor might prescribe different medications known as co-analgesics which specifically treat nerve pain. To preserve muscle strength and protect the patient’s range of motion, the doctor will refer them to physical therapist or rehabilitation therapy. The therapist must be careful though, because research has found that in most cases, muscle strengthening exercises will worsen the pain. The last step a doctor could take, if nothing else has worked, would be a surgical approach. The surgery might involve a nerve graft, or tendon transfer.
What is the prognosis?
The prognosis for Parsonage-Turner Syndrome varies from case to case but typically some patients fully recover and never have another episode, but in most cases, the patient regains around 70%-90% of their function and strength. There is always a small risk that the syndrome will recur but as previously stated, there are some patients that only experience one episode. The patients that have the syndrome affecting both sides of their bodies are more likely to have another episode and less likely to regain their full function and strength.
Back & Spine
-
Degenerative Disk Syndrome
This is information from the Spine-health website; a link to the full article will be linked below.
“Degenerative disc disease is one of the most common causes of low back pain and neck pain, and also one of the most misunderstood. Simply put, this condition is described as the symptoms of pain and possibly radiating weakness or numbness coming from a degenerated disc in the spine. While the definition sounds simple, many patients diagnosed with degenerative disc disease are left wondering exactly what this diagnosis means for them.”
Common Symptoms of Degenerative Disc Disease
There are several symptoms that are fairly consistent for people with lower back pain or neck pain from degenerative disc disease, including:
- Pain that is usually connected to activity and will intensify up at times and then return to a low-grade pain level
- The amount of chronic pain is quite fluctuating between individuals and can be from no pain/just a nagging level of irritation, to severe and crippling pain
- Severe experiences of back or neck pain that can last from a few days to a few months before going back to the individual’s baseline level of chronic pain
- Activities that involve bending, lifting, and twisting will usually make the patient’s pain worse
-Spine-health
As stated above, all of the information is from the Spine-health website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
Sacroiliac Joint Dysfunction
This is information from the Spine-health website; a link to the full article will be linked below.
“Dysfunction in the sacroiliac joint, or SI joint, is thought to cause low back and/or leg pain. The leg pain can be particularly difficult, and may feel similar to sciatica or pain caused by a lumbar disc herniation.
The sacroiliac joint lies next to the bottom of the spine, below the lumbar spine and above the tailbone (coccyx). It connects the sacrum (the triangular bone at the bottom of the spine) with the pelvis (iliac crest). ”
-Dr. Steven G. Yeomans, DCGetting an Accurate Diagnosis
Pinpointing this condition can sometimes be difficult because the symptoms of this condition mimic other conditions. For example, facet syndrome and other lumbar spine conditions including disc herniation and radiculopathy (pain along the sciatic nerve that radiates down the leg). A diagnosis is usually pinpointed by doing a couple of things:
- Physical Examination: your doctor may try to determine if the sacroiliac joint is the cause of pain simply by moving it. If that movement triggers the pain and no other symptoms trigger the pain, that may indicate the SI joint is the problem.
- An Injection to block pain: It takes a highly skilled and experienced physician to be able to insert a needle into the correct portion of the sacroiliac joint. Because of this, the injection is usually guided by X-ray to make sure the joint is properly injected. Sometimes a dye is injected so that the joint is better visualized, which is called an arthrogram.
-Spine-health
As stated above, all of the information is from the Sine-health website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
Scoliosis
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“Scoliosis is a sideways curvature of the spine that occurs most often during the growth spurt just before puberty. While scoliosis can be caused by conditions such as cerebral palsy and muscular dystrophy, the cause of most scoliosis is unknown. Most cases of scoliosis are mild, but some children develop spine deformities that continue to get more severe as they grow. Severe scoliosis can be disabling. An especially severe spinal curve can reduce the amount of space within the chest, making it difficult for the lungs to function properly.”
-Mayo ClinicRecognizing Scoliosis
- Signs and symptoms of scoliosis may include:
- Uneven shoulders
- One shoulder blade that appears more prominent than the other
- Uneven waist
- One hip higher than the other
If a scoliosis curve gets worse, the spine will also rotate or twist, in addition to curving side to side. This causes the ribs on one side of the body to stick out farther than on the other side.
-Mayo Clinic
As stated above, all of the information is from the Mayo Clinic website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT - Signs and symptoms of scoliosis may include:
-
Winged Scapula
This is information from the Washington University School of Medicine website; a link to the full article will be linked below.
Winged scapula is characterized by the shoulder blade abnormally sticking out in the back. A main potential cause for this injury is compression or injury to the long thoracic nerve. The resulting injury of a winged scapula can be painful due to the decreased ability to shrug the shoulder.
As stated above, all of the information is from the Washington University School of Medicine’s website. You can read the full article by following the following link:
VIEW IT
Elbow
-
Little League Elbow
This is information from the HealthyChildren.org website; a link to the full article will be linked below.
“Little League elbow is a common injury (ages 8-17) that is associated with overuse of the particular joint. Most commonly found in pitchers, this injury can also affect catchers, infielders and outfielders. This injury results from having repetitive stress on the inner part of the elbow’s growth plate. The greatest stress occurs during the acceleration phase of throwing a baseball. So, why is this called “little league elbow” if it can affect teenagers? Growing bones are easily injured because the growth plate is much weaker than the ligaments and tendons that surround it. Once the growth plate is fused, athletes are more likely to injure ligaments and tendons instead.”
-HealthyChildren.orgSymptoms
Little League elbow usually progresses gradually and does not have a specific injury, sometimes a distinct “pop” may be felt or other symptoms like:
- Aching
- Sharp Pains
- Inner Elbow Swelling
-HealthChildren.org
As stated above, all of the information is from the Health-Children website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
Radial Head Elbow
This is information from the Joint Paint Expert website; a link to the full article will be linked below.
“Radial head fracture is a fracture of the upper end of the radius bone where it articulates with the lower end of the humerus bone. It can result from falling on an arm or hand that is fully extended, or it can occur with dislocation of the elbow. It can be classified into three types
- Type 1 are undisplaced or minimally displaced fractures (less than 2mm or 1/4th diameter of the neck)
- Type 2 are partially displaced fractures (more than 2mm or 1/4th the diameter of the neck)
- Type 3 are comminuted fractures (multiple fracture fragments)”
–Joint Pain Expert
Symptoms
- History of trauma
- Pain in the outer aspect of the elbow joint
- Mild swelling may be present
- Movements of the elbow joint may be painful and limited
- Wrist pain may be present (indicates a Essex-Lopresti injury)
- Type 1 fracture may present as elbow pain only without any swelling.
-Joint Pain Expert
VIEW IT -
Tennis Elbow
This is information from the Sports Injury Clinic website; a link to the full article will be linked below.
“Tennis elbow (medical term lateral epicondylitis) is a common injury that causes pain on the outside of the elbow. Despite it’s name, this condition is not only seen in tennis players but is also seen in other sports or recreational activities that involve repetitive stress on the muscles around the elbow, such as heavy lifting or decorating. The injury can be very troublesome to treat, especially if it becomes chronic, so it is very important to obtain an accurate diagnosis as early as possible. Tennis elbow can either develop very suddenly (acute) or over a period of days/weeks and more gradually (chronic).”
-Sports Injury ClinicSymptoms
- Pain about 1 to 2 cm down from the bony part on the outside of the elbow, known as the lateral epicondyle.
- Also, there may be associated weakness in the muscles around the forearm and wrist and this may cause difficulty in performing simple tasks such as opening a door handle or shaking hands with someone.
- A doctor or professional therapist may perform a number of assessment tests to help diagnose lateral epicondylitis.
-Sports Injury Clinic
As stated above, all of the information is from the Joint Paint Expert website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
Golfer’s Elbow
This is information from the Mayo Clinic’s website; a link to the full article will be linked below.
Golfer’s elbow refers to the pain that occurs where the flexor muscles of your forearm attach to the inside of your elbow. The pain may also spread down the forearm and into the wrist. This type of pain can be seen in all types of patients who repeatedly use their wrist or fingers, regardless if they play golf or not. Symptoms include: numbness or tingling sensation radiating into the fingers, stiff elbow, weak hand or wrist, and pain or tenderness on the inside of the elbow.
VIEW IT
-Mayo Clinic
Hand + Wrist
-
Carpal Tunnel Syndrome
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“The carpal tunnel is a small channel on the palm side of the wrist. When the nerve in the carpal tunnel is compressed is when the numbness, tingling, and weak handedness occurs often seen in carpal tunnel syndrome. Carpal tunnel can be helped through proper treatment in preventing tingling and numbness and in regaining strength in the wrist.” -Mayo Clinic
VIEW IT
Hip + Upper Leg
-
Hip Replacement Surgery
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“First performed in 1960, hip replacement surgery is one of the most successful operations in all of medicine. Determining if you are a candidate will be an easy decision that your doctor can help you make. If you are struggling from hip pain due to arthritis, a hip fracture, or any other conditions, your everyday activities, like standing out of a chair, might be painful and difficult. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.”
VIEW IT
-AAOS.org13 Things to Know Before Your Hip Replacement
According to an article in U.S. Health News, written by Lisa Esposito, 300,000 hip replacements take place each year. It could drastically improve your lifestyle if you are suffering from the symptoms, but first read over the first few of her “thirteen things you should know.”
- It’s not just an operation for seniors
- How to choose the right surgeon
- Pick a tried-and-true device
- One hip at a time
If you would like to continue reading the article, please follow the link below:
VIEW IT -
Torn Gluteal
This is information from the PhisioAdvisor website; a link to the full article will be linked below.
“This is a rare condition that is characterized by tearing one or more of the gluteal (buttock) muscles. The three gluteal muscles include the gluteus maximus, the gluteus medius, and the gluteus minimus. These muscles begin at the pelvis and extend into the thigh bone. These muscles are used when running, jumping, squatting, and lunging; therefore when there is too much force or repetition being used during these movements, they can tear.” -PhisioAdvisor
VIEW IT -
Sock Aid + Mobility Aid
This is information from the Sock-Aid website; a link to the full article will be linked below.
“With its innovative and unique design, this sock assist aid is unlike any other sock aid or assistant on the market. Where otheraidscan be awkward and clumsy to use, sometimes not even succeeding in helping you, Sock Aid® has been designed to bring efficient support to anyone with mobility problems. Even without the use of both hands, this product will bring back the simplicity of wearing your socks. One simple step and they are on, one swift movement and they are off.” -Sock Aid
VIEW IT -
Trochanteric Bursitis
This is information from the Medscape website; a link to the full article will be linked below.
“This injury is characterized by painful inflammation of the bursa located just above the greater trochanter of the femur. This injury usually occurs when running, after a fall or physical contact, and after hip surgery. A common sign of this injury is hip pain, even though the hip is not directly involved.” -Medscape
VIEW IT
Knee
-
ACL Surgery
Anterior Cruciate Ligament (ACL)
Surgical Repair Videos
To view surgical repair videos regarding the ACL, please follow the link below. You will be asked to “Sign In” to view the video; once prompted, enter this information:
email address: sabrina@myproimpact.com
password: myproimpact -
Shin Splints
This is information from the Houston Methodist website; a link to the full article will be linked below.
“Pain along the front or inside edge of the shin bone (tibia) is commonly referred to as a shin splint, and it is very common in athletes who excessively run and jump. Shin splints on the front of the tibia are referred to as anterior shin splints, and those that occur on the inside of the tibia are called posterior shin splints. They are caused by doing too much, too quickly.” -Houston Methodist
Symptoms
What do shin splints feel like?
- Dull, aching pain is felt where the involved tibialis muscle attaches to the tibia. Redness and swelling can also occur in this area. Tenderness is felt where the muscle attaches to the bone.
- Anterior shin splints are usually felt on the front of the tibia, especially when using the anterior tibialis muscle to bend your foot upward.
- Posterior shin splints produce symptoms along the inside edge of the lower leg. Small bumps may also be felt along the edge of the tibia in this area.
-
Osgood-Schlatter’s Disease
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“The cruciate ligaments are strong bands of tissue that connect the thighbone to the shinbone. The anterior and posterior cruciate ligaments form an “X” in the center of the knee. A PCL injury causes less pain and disability than an ACL tear, but can still sideline an athlete for several weeks or months.” Mayo Clinic
VIEW ITWhat are the symptoms?
This information is from the Mayo Clinic website; a link to the full article will be linked below.
- Pain. Mild to moderate pain in the knee can cause a slight limp or difficulty walking.
- Swelling. Knee swelling occurs rapidly, within hours of the injury.
- Instability. Your knee may feel loose, as if it’s going to give way.
-
Patella Baja vs Alta
This is information from the Radiopaedia website; a link to the full article will be linked below.
“Patella Baja also called patella infera is when the patella is lower than where it should be. A low range of motion and pain is often associated and requires surgery to repair the condition.” -Radiopaedia
VIEW ITThis is information from the Health Fix It website; a link to the full article will be linked below.
“Patella alta is when the patella is located higher that its normal position. Reoccurring dislocation and pain often occurs with patella alta and surgery is necessary in order to correct the problem.” -Health Fix It
VIEW IT -
Patellar Tendonitis
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“Patellar tendonitis is an injury to the tendon connecting your kneecap to your shinbone. It works with the muscles at the front of the thigh and helps you extend your knee so you can run, kick, and jump. Tendonitis in the patella is often called jumper’s knee, and is most common in basketball and volleyball players.” Mayo Clinic
VIEW ITWhat Symptoms will Patellar Tendonitis provide?
This information is from the Mayo Clinic website; a link to the full article will be linked below.
- Pain is the first symptom of patellar tendinitis, usually between your kneecap and where the tendon attaches to your shinbone (tibia).
- At first be present only as you begin physical activity or just after an intense workout
- Eventually interfere with daily movements such as climbing stairs or rising from a chair
-
Patellofemoral Pain Syndrome
This is information from the Mayo Clinic website; a link to the full article will be linked below.
“The kneecap or patella is a small, triangular bone in the front of your knee that moves with the knee as it flexes. It glides up and down along a track at the end of the thighbone (femur) and gives the front thigh muscles (quadriceps) extra leverage for straightening the leg. The patella also protects the other bones in the knee against collisions and falls..” Mayo Clinic
VIEW ITCommon Symptoms
This information is from the AAOS website; a link to the full article will be linked below.
- Pain during exercise and activities that repeatedly bend the knee, such as climbing stairs, running, jumping, or squatting.
- Pain after sitting for a long period of time with your knees bent, such as one does in a movie theater or when riding on an airplane.
- Pain related to a change in activity level or intensity, playing surface, or equipment.
-
PLICA
This is information from the E-Pain Assist website; a link to the full article will be linked below.
“The synovial plica is the inward folds of the synovial lining present in the knee joint capsule. The common region where the plica is present is the inside border of kneecap. The medial suprapatellar plica of the knee is one of the commonest causes of knee pain. About 50% of the patients presenting with knee pain have some amount of irritation of their patellofemoral joint. Medial plica syndrome is present in both young and old patients who are physically very active.” E-Pain Assist
VIEW ITWhat Causes Synovial Plica Irritation?
This information is from the E-Pain Assist website; a link to the full article will be linked below.
- Dysfunction of the patellofemoral joint due to overuse, injury or abnormal mechanics.
- Direct trauma to the knee such as dashboard injuries or falling onto a flexed knee or twisting injuries and overuse of the joint may cause irritation.
- Other knee joint conditions such as a meniscal tear or arthritis could also result in plica irritation.
- Anything that causes bleeding in the joint or synovitis can also lead to plica irritation.
VIEW IT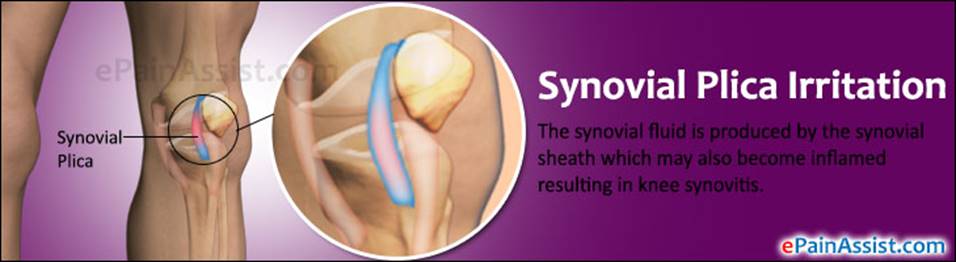
-
Total Knee Replacement
This is information from the Arthritis-health website; a link to the full article will be linked below.
“The goal of total knee replacement surgery is to relieve knee pain and increase knee function by resurfacing the bones that meet at the knee joint. The surgeon removes damaged portions of bone at the end of the femur (thigh-bone) and top of the tibia (shin-bone) and replaces them with prosthetic components. Some surgeries also resurface the back of the patella, or kneecap.” Arthritis-health
VIEW ITWhy a Knee Replacement is Performed
This information is from the Mayo Clinic website; a link to the full article will be linked below.
- Relieve Severe Pain Caused by Osteoarthritis
- Problems with Walking
- Difficulty Climbing Stairs or Getting Out of Chairs
- Moderate or Severe Pain at Rest
-
Jumper’s Knee
This is information from the Mayo Clinic’s website; a link to the full article will be linked below.
Patellar tendinitis, also known as Jumper’s Knee, refers to the injury of the patellar tendon. The patellar tendon extends from the knee cap to the shin and helps to extend the knee. Overuse and excessive stress on the patellar tendon is the usual cause of this injury, and pain is typically the first symptom. This excessive stress can cause small tears within the tendon.
VIEW IT
-Mayo Clinic -
Your posterior cruciate ligament, or PCL, is one of four ligaments in your knee that help stabilizes the joint. The PCL prevents your lower leg bone, or tibia, from sliding back too far on your thighbone (femur). Injuries to the PCL are much less common than other injuries, like ACL tears, and are often the result of a traumatic force on the knee.1,2
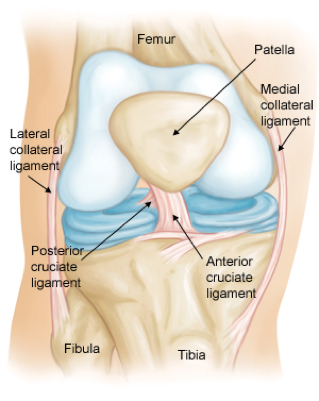 There are three grades of PCL sprains – grade 1, which is a slight stretch, but still allows the PCL to do its job; grade 2, which is a stretch to the point that the ligament is loose; or grade 3, which means the ligament has been completely torn. Grade 3 sprains may cause the knee to be unstable.1
There are three grades of PCL sprains – grade 1, which is a slight stretch, but still allows the PCL to do its job; grade 2, which is a stretch to the point that the ligament is loose; or grade 3, which means the ligament has been completely torn. Grade 3 sprains may cause the knee to be unstable.1Unlike other sprains, PCL sprains are not typically complete. Often, the PCL suffers a grade 1 or 2 tear and is able to repair itself without surgical intervention.1,2 Athletes returning to sports after this injury may do so without issues. Physical therapy can help to strengthen the muscles around the knee, particularly the quadriceps, and provide stabilization through strength while the ligament heals.1,2
Your knee will likely be painful after a PCL injury, and your physician may provide a brace or crutches. Common symptoms of this injury involve swelling, difficulty walking and feeling like your knee is unstable. Injuries to the PCL alone may not require surgery. Compound injuries involving other ligaments or a meniscus, however, may lead to surgery to repair the damaged tissues. The PCL is then rebuilt with arthroscopic surgery and a physical therapy program is started within a few days.1,2
Recovery timelines will depend on your level of physical activity but may last from 6 months to a year or longer, depending on the damage that occurred.1
References 1 and 2 are listed below, respectively.
VIEW IT VIEW ITWhat are the symptoms?
This information is from the Mayo Clinic website; a link to the full article will be linked below.
- Pain. Mild to moderate pain in the knee can cause a slight limp or difficulty walking.
- Swelling. Knee swelling occurs rapidly, within hours of the injury.
- Instability. Your knee may feel loose, as if it’s going to give way.
-
Deep Vein Thrombosis (Signs & Treatment Post Surgery)
This is information from the OrthoInfo website; a link to the full article will be linked below.
Deep Vein Thrombosis (DVT) occurs when a blood clot forms in a deep vein of the body. DVT’s most commonly occur in the legs and a risk factor includes having arthroscopic surgery of the knee or hip. Although relatively uncommon in patients following arthroscopic surgery of the leg, a DVT may lead to a pulmonary embolism which causes the heart and lungs to fail and may result in death. Some signs of a DVT include: swelling, pain or tenderness, distended veins, red or discolored skin, and a firmness of the vein like a “cord”. Signs of pulmonary embolism include shortness of breath, coughing, sudden onset of chest pain, and spitting up blood. If you experience any of these symptoms, contact your physician immediately. In order to diagnose a DVT, Duplex ultrasound is used, which allows doctors to be able to see the blood flow throughout your body. Participation in physical therapy and early movement following surgery have shown to decrease the risks of developing DVT’s by improving blood flow through the veins of your legs and body. Using graded elastic compression socks or compression devices following surgery may also promote blood flow to the legs and prevent DVT’s. Your doctor may prescribe blood thinners, called anticoagulants, to decrease the risk of a DVT or to treat a developed DVT. Posted below are additional resources on information about DVT’s following arthroscopic surgery.
VIEW IT
Lower Leg
-
Exertional Compartment Syndrome
Chronic (Exertional) Compartment syndrome is a condition that is exercise induced. This condition effects outer limbs of the body such as arms and legs.
Chronic (exertional) compartment syndrome develops as an exercised induced condition. More often than not, the individuals that develop this condition are athletes that take part in sports that require strenuous repetitive motions. A few sports that fit into this category are biking, swimming, and running. Younger athletes are the ones who are largely impacted. Chronic compartment syndrome can often be helped by discontinuing the exercise or activity where the condition is thought to come from.
Although the exact cause of exertional compartment syndrome is not completely understood, there are some very good theories. When an individual exercises normally, the muscles will expand in volume. With exertional compartment syndrome, the tissue that surrounds the muscles will not expand with exercise. Due to the lack of expansion, this will lead to pain and a sense of pressure of the affected area.
Symptoms of compartment syndrome can be associated with multiple signs.
- Tightness in the effected limb
- Aching, burning, tingling sensation or numbness in a concentrated area
- Weakness of the affected area
- Often occurs in the same area in both legs
- Swelling or bulging resulting in increased pain
Diagnosing and treating the condition is different depending on the severity of the compartment syndrome. For Chronic compartment syndrome, there are two options if the doctors concluded though X-ray’s that the condition exists. Physical therapy is the first and most common prescription from doctors, but this tends to only provide a short relief from the pain and troubles involved with the syndrome. The second option is a surgical procedure that is called a fasciotomy. This procedure is the leading advancement in treating exertional compartment syndrome. Fasciotomy helps reduce and relives the pressure on the muscles.
Sources of article information are linked below…
VIEW IT VIEW IT -
Pes Anserine Bursitis
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“It is an inflammation of the bursa located between the shinbone, and the three tendons of the hamstring at the inside of the knee. This injury develops due to overuse, and is very common in athletes, especially runners. Symptoms of this injury usually include pain and tenderness approximately 2 to 3 inches below the knee joint. ” -AAOS
VIEW IT -
Shin Splints
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“A sprain or tear in the anterior cruciate ligament (or ACL) is one of the most common knee injuries. This injury is most commonly found occurring in sports like soccer, football, and basketball because they are high demand, quickly moving sports. If you have injured your anterior cruciate ligament, you may require surgery to regain full function of your knee. This will depend on several factors, such as the severity of your injury and your activity level.”
Risk Factors
The anterior cruciate ligament can be injured in numerous ways:
- Quick change in direction
- Stopping very suddenly
- Slowing down while you are running
- Direct contact or impact (a football tackle)
-
Lower extremity Compartment Syndrome
This is information from the Academy of Orthopaedic Surgeons website; a link to the full article will be linked below.
“Compartment syndrome is when an increased amount of pressure builds up in the muscle decreasing blood flow that provides nourishment and oxygen to the muscles. Acute compartment syndrome is dangerous and requires medical attention. It usually is caused by a break in the bone or some type of trauma. Chronic compartment syndrome is not near as serious and is usually caused by repetitive exercise, such as running. If a high pressure remains in the lower part of the body, see a doctor.” -AAOS
VIEW IT -
Sever’s Disease
“Sever’s disease is mainly a cause of heel pain in kids affecting active children aged 8 to 15 years old. Pain at the back of the heel from overuse that if managed correctly, is something the young athlete should grow out of. Rest is an essential part of treatment along with ice or cold therapy and managing training loads.”
Symptoms:
“The main symptom of Sever’s disease is pain and tenderness at the back of the heel which is made worse with physical activity.”
Causes:
“Severs disease is often associated with a rapid growth spurt. As the bones get longer, the muscles and tendons become tighter as they cannot keep up with the bone growth.”
Treatment:
“The aim of treatment is to reduce the pain and inflammation when gently stretch the muscles.”
For more information visit the link below:
VIEW IT
Foot + Ankle
-
Jones Fracture
This is information from the Johns Hopkins Medicine website; a link to the full article will be linked below.
“Occipital neuralgia can originate on its own or from a pinched nerve. Shooting or tingling pain on the side of the scalp or toward one eye and migraines in the back of the head are symptoms often associated with occipital neuralgia. ” -Johns Hopkins
VIEW IT -
Lateral Ankle
This is information from the Sports Injury Clinic website; a link to the full article will be linked below.
“A sprained ankle is one of the most common sports injuries and is also the most frequently re-injured. In the majority of cases the ankle rolls inwards (inversion) under the weight of the rest of the body, resulting in damage to the ligaments on the outside of the ankle. Here you will find everything you need to know about diagnosing, treating and rehabilitating a sprained ankle for an effective and speedy recovery.”
Symptoms
- Pain is usually felt around the ankle joint itself although more specifically on the outside of the ankle where the damaged ligaments are located. Swelling or bruising may present immediately or may take up to 48 hours to develop (depending on the types of structures damaged and the severity of the sprain). It should also be noted that in milder cases, this may never appear at all.
- Sprains are graded 1, 2 or 3 depending on their severity and a professional therapist will be able to tell you which grade of injury you have sustained after carrying out a full ankle assessment. This assessment will include a number of movement, muscle and ligament tests in order determine which structures have been injured and how badly.
As stated above, all of the information is from the Sports Injury Clinic website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
Plantar Fasciitis
This is information from the WebMD website; a link to the full article will be linked below.
“Plantar Fasciitis is the most common cause of heel pain. The plantar fascia is the flat band of tissue (ligament) that connects your heel bone to your toes. It supports the arch of your foot. If you strain your plantar fascia, it gets weak, swollen, and irritated (inflamed). Then your heel or the bottom of your foot hurts when you stand or walk. Plantar fasciitis is common in middle-aged people. It also occurs in younger people who are on their feet a lot, like athletes or soldiers. It can happen in one foot or both feet.”
Symptoms
Plantar fasciitis is caused by straining the ligament that supports your arch. Repeated strain can cause tiny tears in the ligament. These can lead to pain and swelling. This is more likely to happen if:
-
- You have high arches or flat feet.
- You walk, stand, or run for long periods of time, especially on hard surfaces.
- Your feet roll inward too much when you walk
As stated above, all of the information is from the WebMD website. With this being one of the most common and most commonly misunderstood conditions, we encourage you to visit the full article here:
VIEW IT -
-
Sesmoiditis
This is information from the Very Well website; a link to the full article will be linked below.
“This injury is characterized as inflammation of the tissues surrounding the sesamoid bones which causes significant pain under the ball of the foot, under the big toe joint. The pain is usually felt with every step, as the big toe flexes and weight-bearing increases. ” -Very Well
VIEW IT -
Tarsal Tunnel Syndrome
This is information from the John Hopkins Medicine website; a link to the full article will be linked below.
“The tarsal tunnel is a canal on the inside of the ankle. The tunnel contains arteries, tendons, and nerves that aid in the function of the foot. Tarsal tunnel syndrome is when the tibial nerve, that gives feeling on the bottom of the foot, is compressed causing sharp pain, numbness, or tingling in the foot. There are surgical and nonsurgical treatments for this condition depending on the severity.” -John Hopkins
VIEW IT -
Shoes
There are a lot of injuries we can get in our feet, but a good pair of shoes can help alleviate aches and pains and sometimes prevent certain injuries from ever developing.1 We recommend seeing a trained specialist at a running store that can help size you properly, analyze your walking or running, and help point you towards brands and models that may be a good fit for you. Everybody is different, and your shoes should reflect that!
Make sure your shoes are comfortable in the morning and at night. Feet increase in size throughout the day, so it’s important to make sure the shoe truly fits. Some things to look out for include:
- An appropriate toe box. This means that the ball of your foot should be comfortable in the wide part of the shoe near the toes. This is especially important if you have bunions or any other kind of protrusion on your foot.1 Many shoes are available in wide sizes that allow more room through this area if needed.2
- Enough length to slide a finger between your longest toe and the front of the shoe when you are standing.1
- Any lumps, bumps, or material that rubs and irritates your foot.2
- Comfort in standing, walking and running. Nothing should be squeezed or sliding in the shoe – your foot should sit comfortably.1 Test your new shoes out for 5-10 minutes to make sure they are comfortable beyond the first few steps!
Different shoes are designed for different purposes and are often not suitable for other activities. For example, running shoes have more support and cushion in the back, but more flexibility in the toes. Walking shoes may be designed to bend through the ball of the foot. Cross trainers are suitable for exercise in the gym and other workouts.1 Shoes are designed from lasts that are engineered to cater to specific activities, and are made that way for a reason – trust the experts! If you have foot pain but work in an environment where supportive walking or running shoes are not an option, many brands will have models that are based on sneakers and will provide more support while still looking professional.1 These are good options for the work day – good foot support is important all the time!
You may need to use an orthotic to provide extra support for your shoe. Make sure that your orthotic, which should be fitted by a trained professional, fits comfortably in your shoe before you take it home. You should be able to adjust the tightness of your shoe with laces or straps, and the shoe should be well constructed enough that you are not able to easily bend or twist it.1
You will need to replace your shoes on a regular basis. Depending on how often you wear them, and what kind of activity they are for, you may need to replace them anywhere from 6 months to a year after buying them.1
References 1 and 2 are linked below, respectively.
VIEW IT VIEW IT -
Flat Feet
“Flat feet” (pes planus)
Flat feet occur when the entire sole of your foot touches the floor when you’re standing.1 The official name is “pes planus,” but you may also hear the condition referred to as pronated feet or falling arches.2 This can happen after an injury, but some people are just born with flat arches.1 This is common in children and is considered normal until approximately age 10. The bones, ligaments, and muscles of the foot must develop and become able to support an arch.2 Many adults with fallen arches have no pain and no symptoms, but “flat feet” change the way that your legs line up and may cause knee or ankle problems. 1
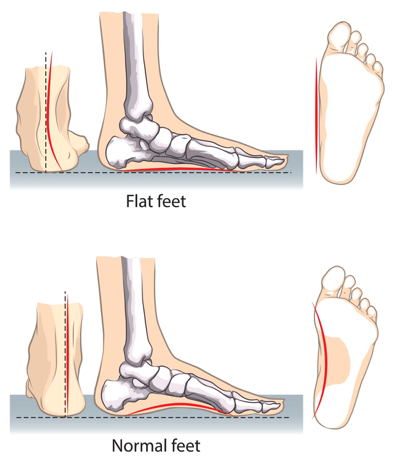
If you’re not having any symptoms from your feet, you may not need to make any changes. If you are having pain in your feet or elsewhere, interventions to improve your pain may include the use of an orthotic, supportive shoes, and physical therapy to address orthopedic concerns. The orthotic and shoes may support your arch, while physical therapy works to strengthen the intrinsic muscles of your foot to strengthen the arch. It most likely will not require surgery for treatment.1,2
You may be at a higher risk for flat feet if you have diabetes or rheumatoid arthritis, are overweight or obese, or have previously injured your feet.1 The appropriate interventions for you may change depending on whether you were born with fallen arches, acquired flat feet from an injury, or developed them slowly over time in adulthood.2
References 1 and 2 are linked below, respectively.
VIEW IT VIEW IT -
Retrocalcaneal Bursitis
What is it?
Retrocalcaneal Bursitis is when the bursa at the back of the heel becomes inflamed from repetitive friction or pressure. The bursa is a small, fluid-filled sac that sits between the heel bone and where the Achilles tendon inserts. It provides cushioning at the back of the heel and allows the Achilles tendon to glide over the heel smoothly. Whenever there is repetitive friction or pressure, the bursa inflames which leads to pain and swelling at the back of the heel. Retrocalcaneal Bursitis is often associated with heel bone spurs.
What causes it?
There are several causes of Retrocalcaneal Bursitis. Over-training in jumping, running, running uphill is a common cause. When high heels are worn, the calf muscle is shortened, resulting in tightness of the Achilles tendon. Changing out of high heels to flat shoes causes excessive pressure on the retrocalcaneal bursa leading to pain. The most common cause of retrocalcaneal bursitis is from ill-fitting shoes and also been linked with gout, arthritis, and fibromyalgia. Typical symptoms of Retrocalcaneal Bursitis are severe pain and swelling in the heel, tenderness to the touch of the heel, cracking sound when the foot is flexed, pain when leaning on heel or sitting with heels on the ground, and increased pain when running, walking, calf raises, etc. To alleviate some of the pain, application of ice pack daily is highly recommended along with taking anti-inflammatory medicine. A corticosteroid injection may be required to stimulate the healing response.
The treatment plan
For treatment, recommendation to a physical therapist is most common. Pain relief and protection are the first step in the healing process. Being able to manage the swelling through icing and other treatment tools is essential. After the inflammation and pain have improved, the next step is to restore normal range of motion along with strength. Increasing endurance and strength of the muscles of the foot and calves will reduce the likelihood of fatigued, weary muscles. After this is achieved, the next desired goal is to get back to daily activities without pain. Following treatment will require prevention of a recurrence, so knowing the causes of retrocalcaneal bursitis is key to prevent recurrence. If symptoms do not go away and the pain is no longer bearable, surgery to remove the bursa can be done, although it most commonly is avoided.
Nerve Pain
-
Suboccipital Neuralgia
This is information from the I Walk Free website; a link to the full article will be linked below.
“Also known as a fifth metatarsal fracture, the Jones Fracture is an injury that affects the outside of the foot close to the small toe. This injury is common in overuse and stress in athletes, and may feel like an ankle sprain. Symptoms may include bruising, tenderness, pain on the outside of the foot, difficulty walking, and chronic ache on the outside of the foot. ” -I Walk Free
VIEW IT -
Facial Nerve Palsy
This is information from the New York Times Health Guide website; a link to the full article will be linked below.
“Facial nerve palsy is when a nerve in the skull is damaged causing the muscles in the face to not move properly. The condition can be caused by pressure on the facial nerve resulting from a tumor, HIV infection, Lyme disease, or no noticeable cause. Some symptoms of facial nerve palsy include paralysis, drooping on the face, and abnormal facial movements. It is important to consult a doctor with the onset of these symptoms.” -NY Times
VIEW IT -
Sciatica
This is information from the Mayo Clinic’s website; a link to the full article will be linked below.
The sciatic nerve travels from the lower back region of the body down through the leg. When pain radiates from this nerve, this is known as sciatica. Symptoms include numbness, pain, and possible inflammation and are usually only present on one side of the body.
VIEW IT
-Mayo Clinic -
Parsonage Turner
“Parsonage–Turner syndrome (PTS) is the term used to describe a neuritis involving the brachial plexus, and is also referred to as idiopathic brachial plexopathy or neuralgic amyotrophy. It may present with symptoms of an isolated peripheral nerve lesion, although the pathology is thought to lie more proximally. PTS is a rare disorder that generally involves one upper limb, mostly the axillary nerve, the upper trunk of the brachial plexus, the suprascapular nerve, and the long thoracic nerve are affected.”
Symptoms:
- Sudden, constant, severe shoulder girdle pain
- May extend from hand to trapezius muscle
- Does not change with positions and usually worse at night
- Sensory deficits and muscle weakness
Treatment:
“In addition to medication therapy patients may be referred for physical therapy. During physical therapy the therapist focuses on patient education, upper-extremity ROM, strengthening exercises to maintain periscapular motion and modalities for adjunct pain relief”
For more information please the link below:
VIEW IT -
Charcot Marie Tooth
Charcot Marie Tooth (CMT), also known as Hereditary Motor Sensory Neuropathy (HMSN) or Peroneal Muscular Atrophy, is one of the most common inherited neurological disorders. This disease affects the structure and/or function of nerves or the conduction sheath covering them, slowing down nerve impulses. In addition, there are motor and sensory symptoms associated with the disorder; including but not limited to, weakness in hands/feet, very high or low foot arches, numbness, and pain. Diagnosis of CMT involves a physical exam including muscle testing, observation of walking, and reflex testing. Physical therapy is among many of health professionals that can help improve quality of life in those with CMT by having the capability to improve pain levels and functioning.
For more information on symptoms, diagnosis, or prognosis please visit the link below:
VIEW IT -
Reflex Sympathetic Dystrophy
Also known as Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) is a chronic pain condition that typically occurs secondary to tissue trauma or surgery but can occur with a lack of injury in rarer cases. CRPS occurs in females 3-4 times more than males, in upper extremities more than lower, and usually around 50-70 years of age2. There are two subtypes of CRPS: the more common Type I or reflex sympathetic dystrophy (RSD), and Type II or causalgia. The neuropathic pain associated with CRPS is disproportionate to the stimulus actually occurring to tissues1. At the site of tissue trauma, pain receptors become sensitized to stimuli. Abnormal messages are then transmitted to the brain relaying a message of a constant painful stimulus, resulting in central sensitization and abnormal mapping at the sensory detection center, or somatosensory cortex. In addition, there is an increased sympathetic nervous system activation, which can cause symptoms such as sweating, temperature, and/or hormonal changes2. Other symptoms associated with CRPS include, but are not limited to, limited mobility and strength, pain, redness, and swelling at the site of tissue injury1. Treatment for RSD or CRPS should include an interdisciplinary approach of healthcare providers, including physical therapy to help normalize stimuli and decrease symptoms. Exercises given to help treat CRPS are individualized to the patient and should be performed frequently.
For more information on RSD/CRPS please see the links below:
2. https://www-ncbi-nlm-nih-gov.ezp.slu.edu/books/NBK430719/
-
Erb’s Palsy
Erb’s palsy is a form of brachial plexus palsy. It is named for one of the doctors who first described this condition, Wilhelm Erb.
The brachial plexus is a network of nerves near the neck that give rise to all the nerves of the arm. These nerves provide movement and feeling to the shoulder, arm, hand, and fingers. Palsy means weakness, and brachial plexus birth palsy causes arm weakness and loss of motion. It is often caused when an infant’s neck is stretched to the side during a difficult delivery.
Most infants with brachial plexus birth palsy will recover both movement and feeling in the affected arm, often with daily physical therapy exercises.For more information, please visit the link below.
VIEW IT
Treatment
-
PRP
“Platelet rich plasma, commonly referred to as “PRP”, is human blood that is spun down and separated producing a concentration of platelets above normal values. Platelets are the clotting cells of our blood, but they also have great potential in enhancing healing of muscle, tendon, and ligaments. Studies suggest that growth factors released by platelets recruit reparative cells, may augment tissue repair, and accelerate soft tissue healing.” (https://www.spinemd.com/treatments/platelet-rich-plasma)
Physical therapists play an important role in improving strength, the range of motion, function, etc., but at times the tissue damage present is unable to be resolved with physical therapy alone. With the new technology of PRP, tissue healing in conjunction with physical therapy can yield results individuals are expecting and desire. It is important to remember that often one type of treatment is unable to solely resolve symptoms. Therefore, in order to expect the best results, it is best to addendum a PRP injection with physical therapy. For questions, see the site listed above or ask your doctor.”
-
An Arthroscopy is Not Just a Scope
From the American Academy of Orthopaedic Surgeons (AAOS):
“Arthroscopy is a surgical procedure orthopedic surgeons use to visualize, diagnose, and treat problems inside a joint. The word arthroscopy comes from two Greeks words, “arthro” (joint) and “skopein” (to look). The term literally means “to look within the patient.” In an arthroscopic examination, an orthopedic surgeon makes a small incision in the patient’s skin and then inserts pencil-sized instruments that contain a small lens and lighting system to magnify and illuminate the structures inside the joint. Light is transmitted through fiber optics to the end of the arthroscope that is inserted into the joint.” –Reference Linked Here
Contrary to the belief that arthroscopies, or “scopes” for short, are performed on minimally damaged anatomic structures, these surgeries can correct extensive abnormalities resulting in increased amount of postoperative physical training necessary.
Take this image for example:
 The damage to the cartilage of the knee can be seen at the end of the probe. Despite this surgery being “just a scope,” the damage to the tissue is extensive. While considering an arthroscopic procedure for you or someone else you know, remember that the procedure itself does not identify the amount of structural damage present.
The damage to the cartilage of the knee can be seen at the end of the probe. Despite this surgery being “just a scope,” the damage to the tissue is extensive. While considering an arthroscopic procedure for you or someone else you know, remember that the procedure itself does not identify the amount of structural damage present.
